Associação Portuguesa de Investigação em Cancro
Pioneering project in Portugal shows the potential of self-sampling and reminder strategies in cervical cancer screening
Pioneering project in Portugal shows the potential of self-sampling and reminder strategies in cervical cancer screening
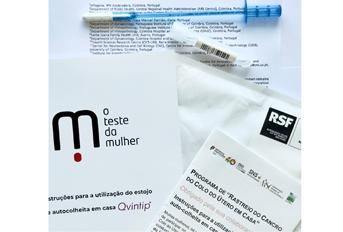
A pioneering study conducted in Central Portugal, by the former ARS Centro in partnership with Infogene, now published in the European Journal of Public Health, showed that integrating HPV self-sampling kits with personalized reminder strategies significantly increased participation among women who had not been screened for more than four years. This approach proved to be an effective and promising strategy to enhance cervical cancer screening coverage and improve early detection of cervical lesions.
Authors and Affiliations:
Sara da Graça Pereira¹, Luís Nobre¹, Marina Ribeiro¹, Patrícia Carvalho², Ana Morais³˒⁴, Rita Sousa³˒⁵, Ana Paula Moniz³˒⁶, Francisco Matos², Graça Fernandes³˒⁷, João Pedro Pimentel²˒³, José Carlos Marinho³˒⁸, José Luís Sá³˒⁵, Olga Ilhéu³˒⁶, Teresa Rebelo³˒⁹, José Fonseca-Moutinho³˒¹⁰, Hugo Prazeres¹, Rui Jorge Nobre¹¹˒¹² , Fernanda Loureiro²˒³
¹ Infogene, IPN Aceleradora, Coimbra, Portugal
² Administração Regional de Saúde do Centro (ARS Centro), Departamento de Saúde Pública, Coimbra, Portugal
³ Grupo de Trabalho do Cancro do Colo do Útero (GTCCU), ARS Centro, Coimbra, Portugal
⁴ USF Salinas, Cacia, Portugal
⁵ Serviço de Ginecologia, Instituto Português de Oncologia de Coimbra, Portugal
⁶ Serviço de Anatomia Patológica, Instituto Português de Oncologia de Coimbra, Portugal
⁷ Serviço de Anatomia Patológica, CHUC, Portugal
⁸ USF Santa Joana, Aveiro, Portugal
⁹ Serviço de Ginecologia, CHUC, Portugal
¹⁰ CICS-UBI, Universidade da Beira Interior, Covilhã, Portugal
¹¹ CNC e CIBB, Universidade de Coimbra, Portugal
¹² Instituto de Investigação Interdisciplinar, Universidade de Coimbra, Portugal
Abstract:
Cervical cancer (CC) screening is essential for reducing its incidence, yet engaging under-screened women remains challenging. Self-sampling has emerged as a promising solution to enhance attendance; however, its integration into programmes has proven difficult. This study evaluated a multimodal approach combining self-sampling, human papillomavirus (HPV) testing, and personalized contact to reach women not attending conventional CC screening. To achieve this, 801 women aged 30–59 who had not participated in Portugal’s Central Region CC screening programme for more than 4 years were selected based on specific criteria. Of these, 114 women were excluded for not meeting eligibility criteria, resulting in 687 eligible participants. Using an ‘opt-in’ approach, women who consented to participate received cervicovaginal self-sampling kits at home. Multiple contact strategies, including phone calls and reminder letters, were employed to encourage participation. Women testing positive for high-risk HPV (hr-HPV) were referred for gynaecological follow-up. Of the eligible women, 307 (44.7%) consented to participate and 198 (28.8%) provided valid samples for hr-HPV testing. Approximately 60.0% of participants were enrolled after the first reminder phone call, while additional contact strategies accounted for one-third of submitted samples. Among 12 hr-HPV positive cases, 11 completed gynaecological follow-up, resulting in the identification of six cervical lesions. This study confirms the feasibility and effectiveness of combining self-sampling, HPV testing, and personalized contact strategies to improve CC screening uptake among under-screened women. The findings highlight the potential of such interventions to address participation gaps and enhance early detection of cervical lesions, ultimately reducing CC incidence.
Journal: European Journal of Public Health (2025)




